Outcomes Advisor™
Dimensional Insight’s Outcomes Advisor provides up-to-date and actionable data on outcomes measures and KPIs for your hospital or health system, as defined by CMS. These include those KPIs used in a variety of pay-for-performance programs.
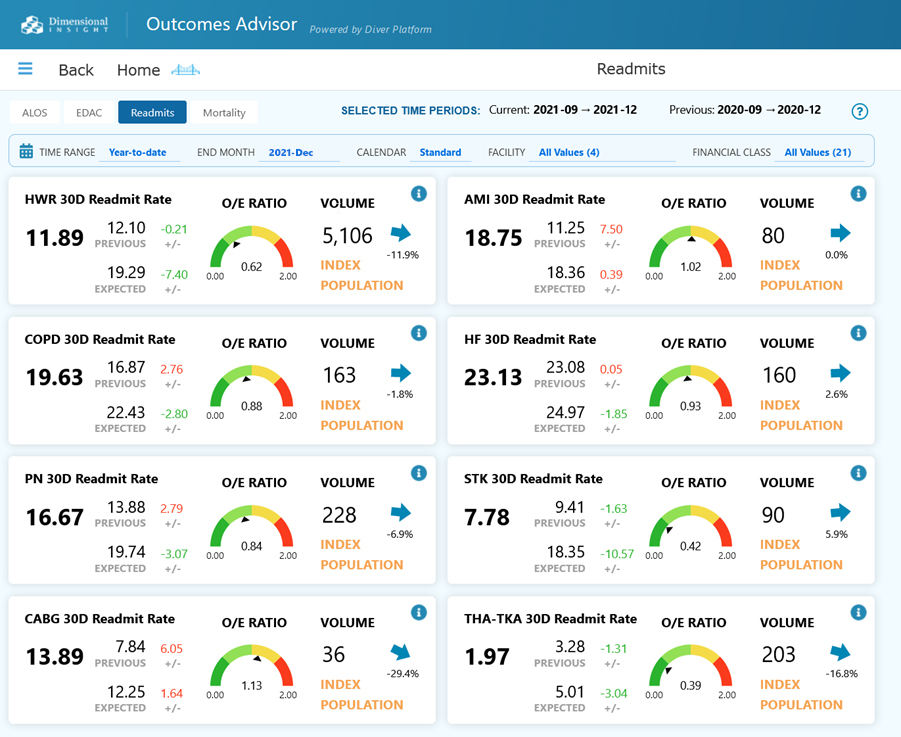
Outcomes Advisor provides quality managers, hospital administrators, and providers with a succinct, intuitive, and actionable perspective on outcomes for a variety of ALOS, mortality, readmissions, and EDAC measures, and a number of IQI, PDI, and PSI measures.
Information is available through dashboards, reports, and ad hoc analytics. Users can view key metrics and then simply click on any number or graphical view to answer questions about the underlying detail.
The solution contains benchmark data from a Medicare claims dataset of more than 3,000 hospitals. Benchmark your performance against a peer group cohort and easily determine areas where you are performing better than or worse than expected. With this information, you can better focus efforts of your limited resources and maximize performance improvement.
Data is updated daily, meaning decision makers can take action to improve performance during a reporting period instead of having to wait until after the period ends and reports from external sources are already published. By then, it is too late and penalties may already be in place. With Outcomes Advisor, you can make decisions when they are still impactful.
Benefits of Outcomes Advisor
Reduce readmissions
A customer cut readmissions by 37%.
Increase revenue
The same customer boosted quality-based reimbursements by $2.5M in two years.
Reduce patient days
Another customer decreased Medicare ALOS by 28.5%.
Access to Industry Standard Out-of-the-Box Measures
Click on the interactive module below to explore our pre-defined measures. With more than 500 standard measures and data elements built into the application, Outcomes Advisor allows you to immediately begin analyzing information without having to build your analytics environment from scratch.
Examples of Outcomes Advisor dashboards:
Part of Dimensional Insight’s Library of Applications
Outcomes Advisor is built on Dimensional Insight’s award-winning enterprise analytics platform and is part of the company’s library of off-the-shelf applications. Deploying these applications results in deep and sustained clinical, financial, and operational improvements that impact patient care and your organization’s bottom line. Diver Platform and Dimensional Insight’s Library of Applications satisfy your health system’s enterprise reporting needs.
Benefits to the Library of Applications approach
Data trust across departments
Data governance ensures the use of consistent, standardized, validated, and documented business rules and measures across applications. This means all departments are using the same definitions for decision-making.
Quick to implement
Dimensional Insight uses a proven process that leads to short implementation times and quick time to value. Applications build on previously implemented Dimensional Insight apps, leading to even shorter deployment times, especially when compared to department-specific apps from multiple vendors.
Lower overall costs
Because Dimensional Insight Applications are all built upon Diver Platform, hospitals do not incur the high costs associated with licensing and supporting solutions from multiple vendors.
Consistent look and feel across application areas
Applications all have a consistent, intuitive look and feel. Moving from one application to another is seamless. Executives and other users do not have to learn several applications.
Designed to be customizable
Users access 1,000s of off-the-shelf industry-standard business rules that can be deployed “as is” or adjusted to your unique requirements.
Built on the award-winning, healthcare enterprise analytics platform: Diver Platform®
8 time Best in KLAS winner from 2010 to 2021
Our customers have perennially rated Diver Platform #1.
Leading edge technology
Enterprise analytics platform combines ETL, data management, and self-service analytics to provide a powerful engine that generates results for all types of users.
Data Governance
Rigorous processes that manage and protect data ensure data trust and consistency across the organization.
Custom development
Since Diver is a development platform, customers can modify existing Dimensional Insight applications or build new ones on their own.
Data when and where you want it
Users can easily access data from their desktop, laptop, tablet, or phone.
Multiple deployment options
Organizations can host deployment on site, in the cloud, or via SaaS.